
Pellegrini-Stieda Disease: Definition, Clinical Features and Treatment
- 21/10/2025
What is Pellegrini–Stieda disease?
Pellegrini–Stieda disease is characterized by post-traumatic ossification or calcification of the medial collateral ligament (MCL), typically at its femoral insertion. On X-ray, it appears as a linear or curved calcification along the medial femoral condyle. When associated with pain, stiffness, or restricted function, it is referred to as the Pellegrini–Stieda syndrome (Contreras, 2003).
What causes Pellegrini–Stieda disease?
The most frequent cause is a valgus knee trauma leading to partial or complete MCL injury, followed by inflammation, fibrosis, and secondary dystrophic ossification. Some cases occur without clear trauma, possibly related to repetitive microtrauma or tissue degeneration (Mabrouk & Sherman, 2025; Restrepo & Molina, 2016). Gokcen et al. (2015) described an intraligamentous dystrophic calcification variant without ligament rupture that mimics this disease radiographically.
What are the symptoms of Pellegrini–Stieda disease?
- Medial knee pain along the course of the MCL.
- Joint stiffness and limited range of motion.
- Local tenderness to palpation.
- Occasionally asymptomatic, discovered incidentally on imaging (Paredes & Sáiz, 2011; Santos et al., 2012).
How is Pellegrini–Stieda disease classified (types)?
The classification describes the shape of the ossification on radiographs:
- Type I: Inferior beak-like ossification attached to the femur.
- Type II: Inferior drop-shaped ossification parallel to the femur.
- Type III: Superior linear ossification parallel to the femur.
- Type IV: Double beak-shaped ossification, superior and inferior (more complex).
Clinical note: The type does not necessarily correlate with symptom severity, but it helps describe radiographic patterns and guide management.

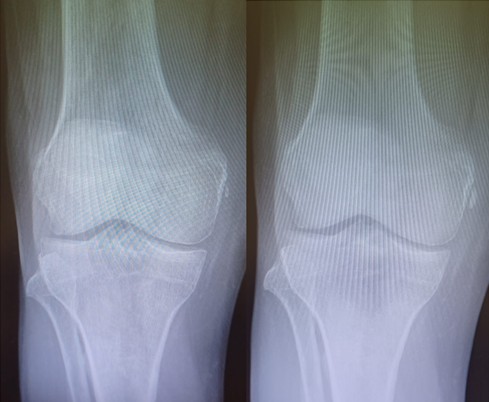
Two examples of Pellegrini–Stieda disease.
How is Pellegrini–Stieda disease diagnosed?
- X-ray: Curved or linear calcifications adjacent to the medial femoral condyle (Panadero et al., 2012).
- MRI: Helps distinguish acute from chronic lesions and assess ligament integrity (Restrepo & Molina, 2016).
- Ultrasound: Identifies calcifications and can guide percutaneous procedures such as lavage (Panadero et al., 2012; Rizky et al., 2023).
What is the initial treatment for Pellegrini–Stieda disease?
- Nonsteroidal anti-inflammatory drugs (NSAIDs).
- Physical therapy to restore range of motion and strengthen muscles.
- Relative rest and activity modification.
- Local corticosteroid injection in selected cases (Contreras, 2003).
Most patients improve within 4–6 months of conservative treatment (Santos et al., 2012).
What is ultrasound-guided lavage?
Ultrasound-guided lavage is a minimally invasive procedure performed by inserting a needle into the calcific deposit under ultrasound guidance to fragment and aspirate the material. Evidence:
- Mabrouk & Sherman (2025): Ultrasound-guided lavage combined with PRP injection is a promising option for refractory cases after failed conservative treatment.
- Rizky et al. (2023): Case reports show significant pain relief and improved mobility within weeks after lavage. Conclusion: a safe, effective, minimally invasive technique for localized calcifications.
When is surgery indicated for Pellegrini–Stieda disease?
Surgical excision is reserved for:
- Persistent, disabling pain.
- Failure of conservative or lavage therapy.
- Compression of adjacent structures or severe mechanical restriction.
Premature surgery (before 6–12 months) is discouraged due to the risk of recurrence (Theivendran et al., 2009).
What is the prognosis of Pellegrini–Stieda disease?
Overall, the prognosis is good. Most cases respond well to conservative treatment. Ultrasound-guided, minimally invasive techniques offer rapid improvement and avoid surgery (Mabrouk & Sherman, 2025; Rizky et al., 2023). Surgical outcomes are also satisfactory in well-selected patients (Theivendran et al., 2009).
Clinical recommendations:
- Start with conservative management.
- Use ultrasound for diagnosis and intervention planning.
- Consider ultrasound-guided lavage ± PRP for localized persistent calcifications.
- Reserve surgery for refractory cases.
- Document clinical and imaging follow-up to monitor recovery or recurrence.
References
- Contreras MA. Pellegrini–Stieda disease. Rev Esp Enferm Metab Oseas. 2003;12:57–58. link
- Gokcen N, Kelle B, Kozanoglu E. Intraligamentous calcification of the medial collateral ligament mimicking Pellegrini–Stieda syndrome. Turk J Phys Med Rehab. 2015;61:70–72. link
- Mabrouk A, Sherman AL. Pellegrini–Stieda Disease. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. PMID: 30570968.
- Panadero F, et al. Pellegrini–Stieda Syndrome. Rev Dig de Ecografía Clínica. Sociedad Española de Ecografía. 2012;3(1):19–20. link
- Paredes F, Sáiz S. Pellegrini–Stieda Disease. FM. 2011;10(6):347–348.
- Restrepo J, Molina M. Pellegrini–Stieda Syndrome: beyond the imaging sign. Rev Colomb Reumatol. 2016;23(3):210–212. link
- Rizky DA, Lee K, Sulaeman WS, Butarbutar JCP, Suginawan ET. Ultrasound-guided percutaneous lavage for Pellegrini–Stieda Syndrome: case report. J Orthop Case Rep. 2023;13(7):27–32. doi:10.13107/jocr.2023.v13.i07.3742. PMID: 37521393.
- Santos J, Ramos L, García D, Bermúdez C. Pellegrini–Stieda Syndrome as a cause of knee pain. Semergen. 2012;38. link
- Theivendran K, Lever E, Hart W. Good outcome following surgical treatment of Pellegrini–Stieda syndrome. Knee Surg Sports Traumatol Arthrosc. 2009;17:1231–1233. DOI: 10.1007/s00167-009-0725-0
Book an appointment with Dr. Jordi Jiménez. He will see you at the Palma de Mallorca clinic and help you recover your quality of life.

![[VIDEO] Ultrasound-Guided Injection for Trigger Finger](https://drjordijimenez.com/imagen/100/100/Imagenes/infiltracion-ecoguidada-dedo-resorte-drjordijimenez.jpg)
![[VIDEO] Ultrasound-guided infiltration of the lumbar facets](https://drjordijimenez.com/imagen/100/100/imagenes-pagina/sindrome-facetario-lumbar-drjordijimenez (1).jpg)
![[VIDEO] Ultrasound-guided infiltration of the hip joint](https://drjordijimenez.com/imagen/100/100/Imagenes/valgo-dinamico-rodilla-drjordijimenez.jpg)