
Plantar fasciitis
- 14/02/2019
What is plantar fasciitis or fasciosis?
Plantar fasciitis is a degenerative process that causes inflammation of the plantar fascia, a structure of elastic connective tissue that connects the calcaneus to the metatarsal area. This inflammation causes pain in the medial part of the heel. It is the most common cause of consultation for heel pain. 10% of the population will experience heel pain throughout their lives. More than 80% of these patients are adults between the ages of 25 and 65.
What are the causes and predisposing factors of plantar fasciitis?
Several factors can cause or contribute to inflammation or degeneration of the plantar fascia.
Factors related to foot biomechanics and gait:
Arch problems: Both having flat feet (low arches) and a very high arch (cavus feet) can alter the way weight is distributed across the foot and increase tension on the plantar fascia.
Tight or shortened Achilles tendon: Tightness in the calf muscles and Achilles tendon can limit ankle dorsiflexion, placing additional pressure on the plantar fascia.
Atypical gait pattern: An inefficient walking or running gait can place additional stress on the fascia.
Activity and lifestyle factors:
Overload or overuse: Activities that place a lot of repetitive pressure on the heel, such as running long distances (especially downhill or on uneven surfaces), dancing, or high-impact sports.
Prolonged standing: Professions that require standing or walking on hard surfaces for long hours (e.g., factory workers, teachers, nurses).
Sudden increase in physical activity: Abruptly changing the level or intensity of exercise without gradual adaptation.
Improper footwear: Wearing shoes that do not provide good arch support, have soft soles, are worn out, or have high heels.
Other risk factors:
Age: It is most common in people between 40 and 60 years of age.
Obesity or overweight: Excess weight puts constant additional pressure on the plantar fascia.
Systemic diseases: Conditions such as rheumatoid arthritis, psoriatic arthritis, or diabetes may increase the risk.
Pregnancy: Weight gain and hormonal changes may contribute to its onset.
What are the main symptoms of plantar fasciitis?
The clinical presentation of plantar fasciitis is characterized by heel pain, predominantly in the morning or after prolonged rest. The pain typically decreases with the start of daily activity and worsens with weight bearing, sports activities, and prolonged walking. It usually presents as a fingertip pain in the most medial part of the heel, coinciding with the insertion of the medial plantar fascia.
How is plantar fasciitis diagnosed?
Not all heel pain is plantar fasciitis, so establishing a prior differential diagnosis is important. The history and physical examination will help us make this differential diagnosis with:
-Neurological pathology:
- Tarsal tunnel syndrome.
- S1 radiculopathy.
- Entrapment of the first branch of the lateral plantar nerve (also called Baxter's nerve).
- Entrapment of the medial calcaneal nerve.
- Peripheral neuropathy.
-Soft tissue pathology:
- Fascial tears.
- Enthesopathies.
- Fat pad atrophy.
- Achilles tendonitis.
- Flexor longus tendonitis.
- Plantar fibromatosis.
- Posterior tibial tendonitis.
-Skeletal pathology:
- Stress fractures of the calcaneus.
- Bone contusion.
- Inflammatory arthropathies.
What tests help diagnose plantar fasciitis?
- A plain X-ray will sometimes reveal a bony growth resulting from prolonged excessive traction on the plantar fascia, a heel spur.
- Ultrasound offers a rapid, inexpensive diagnosis that can be compared with a healthy foot.
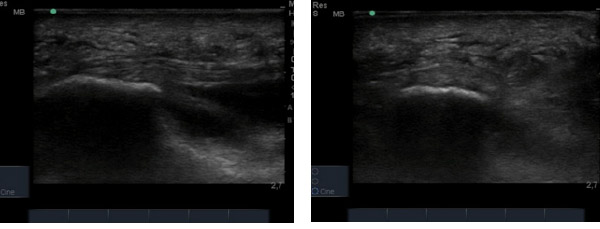
Healthy fascia: longitudinal axis / transverse axis

Diseased fascia: Longitudinal axis / transverse axis fasciitis
Ultrasound examination will show focal thickening at the fascial insertion in the calcaneus (greater than 4-5 mm thick), hypoechoic, with loss of fibrillar pattern, less frequently perifascial effusion, and occasionally cortical irregularities in the calcaneus. Lateral band involvement of the plantar fascia may coexist in patients who overload the external edge of the heel to avoid putting pressure on the painful area.
How is plantar fasciitis treated?
Regarding treatment, it is recommended to avoid wearing flat shoes, correct biomechanical gait abnormalities when present, and perform physical therapy exercises aimed at increasing flexibility and strengthening the muscles in the region (fascial and posterior chain stretching).
See the section on stretching and strengthening exercises for plantar fasciitis and FOOT CORE exercises.
The above measures can be combined with:
- Pharmacological treatment (analgesics and NSAIDs).
- Extracorporeal shock waves
- Perifascial injections of local anesthetic + corticosteroids. One or two injections spaced two to three weeks apart are effective as short-term pain treatment, although their long-term efficacy is not as good.
- Nighttime dorsiflexion splinting of the foot, maintaining constant fascial tension without weight-bearing.
- PRP (platelet-rich plasma) injections are indicated in cases of fasciosis or long-standing fascial defects that require stimulation for regeneration.
- Radiofrequency of the first branch of the lateral plantar nerve.
- Percutaneous intratissue electrolysis (PTE).
Make an appointment with Dr. Jordi Jiménez. He will see you in the center of Palma and help you regain your quality of life.

![[VIDEO] Ultrasound-Guided Injection for Trigger Finger](https://drjordijimenez.com/imagen/100/100/Imagenes/infiltracion-ecoguidada-dedo-resorte-drjordijimenez.jpg)
![[VIDEO] Ultrasound-guided infiltration of the lumbar facets](https://drjordijimenez.com/imagen/100/100/imagenes-pagina/sindrome-facetario-lumbar-drjordijimenez (1).jpg)
![[VIDEO] Ultrasound-guided infiltration of the hip joint](https://drjordijimenez.com/imagen/100/100/Imagenes/valgo-dinamico-rodilla-drjordijimenez.jpg)