Scheuermann's disease
- 28/07/2025
What is Scheuermann's Disease?
Scheuermann's disease is a condition affecting the spine, causing thoracolumbar or dorsal hyperkyphosis (excessive forward curvature of the spine) that often manifests during adolescence. Although it can be a source of concern, especially due to its aesthetic impact and associated pain, a clear understanding of its causes, symptoms, and treatments is essential for effective management.
What causes Scheuermann's Disease?
The exact etiology of Scheuermann's disease is unknown, but it is considered multifactorial. The most recent research suggests a combination of genetic and mechanical factors:
- Genetic Predisposition: There is evidence of familial clustering, suggesting a hereditary component, possibly with an autosomal dominant pattern. High concordance has been observed in monozygotic twins.
- Biomechanical Factors: Excessive mechanical stresses on the spine during growth are thought to play a role. This includes:
- Intense physical activity: The condition is most commonly seen in high-performance athletes who subject their backs to repetitive stress and heavy loads.
- Obesity: Being overweight can increase pressure on the developing spine.
- Repetitive microtrauma: Small injuries or constant stress on the vertebral endplates during growth can contribute to wedging.
What are the symptoms of Scheuermann's disease?
Symptoms of Scheuermann's disease usually appear between the ages of 10 and 16, during a period of rapid growth. The most common include:
- Thoracic hyperkyphosis (rounded back): This is the most visible sign, although its degree can vary. The main characteristic is that this curvature is rigid and does not fully correct when attempting to straighten.
- Back or thoracolumbar pain: Approximately half of patients experience pain, which is usually localized to the area of the deformity (thoracic or thoracolumbar). This pain tends to worsen with physical activity and improves with rest.
- Muscle fatigue: The back muscles may fatigue more easily due to the extra effort required to maintain a posture.
- Rigidity: Limited spinal movement, especially in extension.
How is Scheuermann's disease diagnosed?
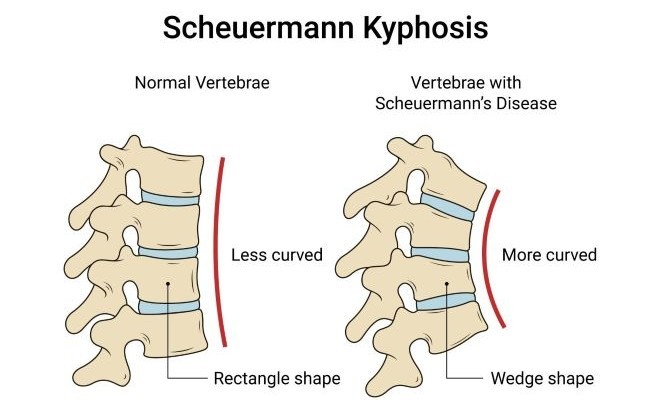
The diagnosis is based on clinical symptoms (symptoms and physical examination) and primarily on spinal x-rays(Figure 1). Radiological criteria include the presence of three or more contiguous vertebrae with anterior wedging of at least 5 degrees, as well as other abnormalities such as Schmorl's nodes (herniations of the intervertebral disc into the vertebral body). A lateral spine teleradiograph with the patient standing is the most commonly used diagnostic projection.

Figure 1
How is Scheuermann's disease treated?
Treatment for Scheuermann's disease varies depending on the severity of the curve, the presence of pain, and the patient's degree of skeletal maturity. Recent publications agree that conservative management is the first line of action.
Conservative Treatment
The main goal is to control pain, correct posture, and prevent the curve from progressing. It includes:
- Physical Therapy and Rehabilitation: Therapeutic exercises: Strengthening the back and abdominal muscles, stretching to improve flexibility and mobility.
- Postural Reeducation: Teaching correct postural habits for daily life.
- Manual Therapy: Massages and mobilizations to reduce muscle tension.
- Corsets or Orthopedic Devices: Especially in growing patients with progressive or more pronounced curves, corsets can be used to help shape the spine and prevent the kyphosis from worsening. The long-term effectiveness of corsets is still under study, but they are considered an important option during the growth phase.
- Medications: Analgesics and anti-inflammatories may be prescribed to relieve pain.
When is surgery necessary for Scheuermann's disease?
Surgery is reserved for specific cases in which conservative treatment has not been effective or when the deformity is severe and causes significant problems:
- Severe kyphosis: Surgery is considered for curves exceeding 70-75 degrees in the thoracic spine or 25-30 degrees in the thoracolumbar spine.
- Intractable pain: When pain is persistent and severe despite conservative therapies.
- Neurological deficit: If the curve is affecting the nerves or spinal cord.
- Cardiorespiratory compromise: In very severe cases where the deformity affects lung or heart function.
- Cosmetic reasons: In some patients, the deformity can be a source of significant psychological distress.
The most common surgery is instrumented posterior fusion, which seeks to correct the curve and fuse the vertebrae to stabilize the spine. Although effective, surgery carries risks. Surgical approaches, whether anterior, posterior, or combined, do not appear to show significant differences in short- or long-term correction, but the posterior-only approach is generally associated with a lower risk of complications and bleeding.
Book an appointment with Dr. Jordi Jiménez. He will see you at the center of Palma de Mallorca and help you regain your quality of life.

![[VIDEO] Ultrasound-Guided Injection for Trigger Finger](https://drjordijimenez.com/imagen/100/100/Imagenes/infiltracion-ecoguidada-dedo-resorte-drjordijimenez.jpg)
![[VIDEO] Ultrasound-guided infiltration of the lumbar facets](https://drjordijimenez.com/imagen/100/100/imagenes-pagina/sindrome-facetario-lumbar-drjordijimenez (1).jpg)
![[VIDEO] Ultrasound-guided infiltration of the hip joint](https://drjordijimenez.com/imagen/100/100/Imagenes/valgo-dinamico-rodilla-drjordijimenez.jpg)