
Thoracic outlet syndrome
- 20/12/2022
What is thoracic outlet syndrome?
Thoracic outlet syndrome is defined as a set of variable clinical signs and symptoms resulting from compression of the brachial plexus, subclavian artery, or vein as they pass through the anatomical passages that carry these structures from the neck to the upper extremity.
How common is thoracic outlet syndrome?
This often underdiagnosed clinical entity has an incidence of 10 cases per 100,000 inhabitants. However, anatomical studies on cadavers suggest that up to 90% of the population have anatomical variants that may determine the presence of this syndrome, with the condition being more common in women (a 4:1 ratio).
Which anatomical areas are involved in thoracic outlet syndrome?
The narrowing of this passage can be acquired or congenital in three specific anatomical areas:
The interscalene triangle, the most medial of the compartments, contains the superior, middle, and inferior trunks of the brachial plexus and the subclavian artery. Anteriorly, it is bounded by the anterior scalene, posteriorly by the middle and posterior scalenes, and inferiorly by the first rib. It is the most common site of neurological compression.
The costoclavicular space, the middle compartment, is the most common site of vascular compression. It is bordered superiorly by the clavicle, anteriorly by the subclavius muscle, and posteriorly by the first rib and the middle scalene muscle.
The lesser retropectoral space, the more lateral compartment, is bordered anteriorly by the pectoralis minor muscle, superiorly by the subscapularis muscle, and inferiorly by the anterior thoracic wall. In this compartment, we find the divisions of the brachial plexus and the axillary vascular bundle.
The anatomical abnormalities that can affect these compartments are:
- Scalene muscle hypertrophy or their insertional variability.
- Presence of the minimal accessory scalene muscle.
- Soft tissue tumors.
- Congenital fibrous bands.
- Anomalous muscle bands.
- Cervical rib.(Figure 2 and 3)
- Prominent C7 transverse processes, bone callus, or abnormalities of the first rib.(Figure 1 and 2)
- Bone tumors.
- Lesions of the sternoclavicular joint.
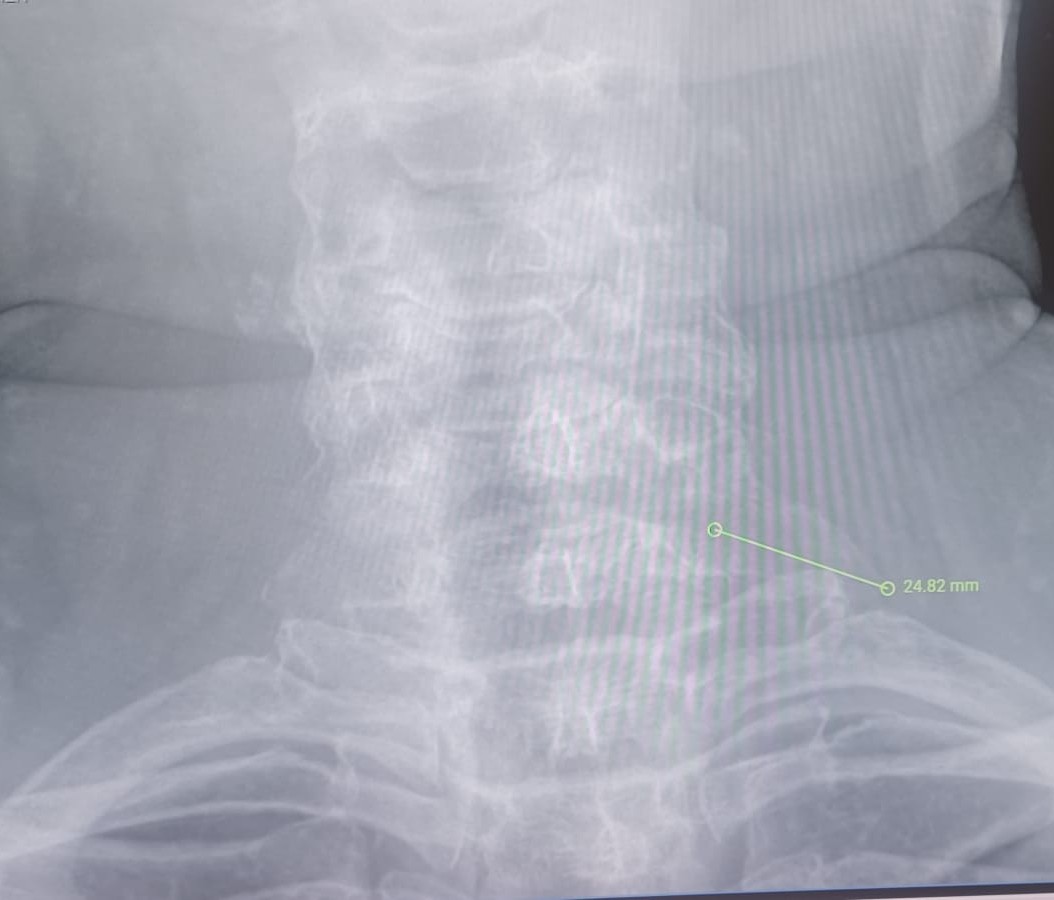
Figure 1: Prominent c7 transverse process

Figure 2: Right cervical rib and prominent left c7 transverse process

Figure 3: Bilateral cervical rib
How is thoracic outlet syndrome classified?
Depending on the affected component, we have:
1. Neurogenic thoracic outlet syndrome:
Due to compression of the brachial plexus. It has two types:
- True or classic, rare, 1 case per million inhabitants. Also known as Gilliat-Summer syndrome, it is characterized by atrophy of the abductor pollicis brevis muscle and the hypothenar and interosseous muscles of the hand.
- Disputed (non-neurogenic), the most common form of thoracic outlet syndrome (accounting for 90-95% of all cases with a prevalence of up to 80 cases per 1,000 population).
2. Arterial thoracic outlet syndrome:
Accounts for 1-5% of all cases, in patients who perform repetitive upper extremity movements with arms raised above the shoulders.
3. Venous thoracic outlet syndrome:
Accounts for 2-3% of cases.
What are the symptoms of thoracic outlet syndrome?
The variability of clinical manifestations and the lack of specific data make the diagnosis of this syndrome a real challenge.
Within neurogenic origins, the symptoms will vary depending on the location of the compression. The most common is in the lower part of the brachial plexus, affecting the C8-T1 roots, which will cause clinical involvement of the ulnar area of the forearm, hand, axillary region, and anterior shoulder. Upper brachial plexus compression will affect the C5-C7 roots, with clinical presentation of insidious supraclavicular pain radiating to the face, head, scapula, or distal involvement of the radial nerve on the back of the second and third fingers.
It is important to perform a differential diagnosis with peripheral neuropathies due to compression (carpal tunnel syndrome, Fröhse's arcade syndrome, etc.) and cervical radiculopathies. It should be remembered that thoracic outlet syndrome typically presents with a broad anatomical distribution of symptoms that do not follow a specific radicular pattern. In thoracic venous outlet syndrome, we find significant pain and edema in the upper extremity with a feeling of heaviness and cyanosis that worsens after physical activity, and in the case of arterial venous outlet syndrome, pain, numbness, coldness, and pallor that worsens at low temperatures.
How is thoracic outlet syndrome diagnosed?
A physical examination of the cervical spine, shoulders, and upper extremities is essential, assessing the patient's head-neck-shoulder position and general posture.
Comparison of the affected limb with the contralateral limb will provide information about temperature, color, muscle atrophy, and trophic changes in the nails. Palpation of the supraclavicular region may reveal tenderness in this area, palpable masses, etc.
There are various exploratory maneuvers that allow us to suspect neurovascular compression and approximate the diagnosis:
- Wright test: Patient seated with arm in hyperabduction and external rotation. Head turned to the side opposite the limb being examined. A decrease in the radial pulse is assessed (this can occur in up to 7% of the healthy population).
- Adson's test: the patient sits with their arm abducted at 30° with their head turned toward the side being examined. Forced and sustained inspiration is requested, which causes elevation of the first rib (floor of the interscalene triangle) and increased tone of the anterior scalene muscle. The radial pulse is simultaneously palpated, and its reduction or elimination is assessed.
- Roos' test: described as the most reliable test for diagnosing thoracic outlet syndrome, especially the neurogenic type. The patient sits with their arms abducted at 90° and their elbows also flexed at 90°. In this position, the patient is asked to open and close their hands for a period of 3 minutes. Patients with thoracic outlet syndrome will report symptoms such as paresthesia, heaviness in the arms, or exacerbation of their usual pain, leading them to refuse to take the test.
What diagnostic tests are ordered for thoracic outlet syndrome?
- Plain X-ray: A cervical X-ray and chest X-ray are a first diagnostic approach that allows us to rule out cervical ribs, prominent transverse processes, bone callus in fractures, degenerative processes of the cervical spine, or neoplasia (Pancoast tumor).
- Electromyography: In many cases, electromyography may be normal, but it can be used to rule out cervical root involvement, brachial plexus injuries, or peripheral neuropathies due to compression.
- Ultrasound: Useful in the evaluation of syndromes with venous and arterial involvement, demonstrating alterations in flow velocity in the presence of stenosis or aneurysms, the presence of venous thrombi, and with the possibility of correlating the patient's symptoms with the ultrasound findings in a dynamic manner. CT arteriography and venography: provide vascular imaging of great diagnostic help in cases of arterial or venous syndrome.
- Magnetic resonance imaging: the test of choice for evaluating brachial plexus compression in neurogenic syndrome.
How is thoracic outlet syndrome treated?
Treatment for thoracic outlet syndrome is usually conservative. Physical therapy is primarily indicated in cases of neurogenic involvement, while surgical treatment is reserved for vascular and neurogenic cases that do not respond to conservative treatment.
Correction of predisposing factors:
In the early stages of the neurogenic form, symptoms may be caused by traction on the lower trunk of the brachial plexus, a condition that worsens due to obesity, poor postural hygiene, or occupational factors.
Conservative treatment aims to improve:
- The normal arthrokinetics of the surrounding joints.
- Correction of muscle weaknesses and imbalances.
- Improve the mobility of nerve structures to avoid compression or tension in the gorge.
Physical therapy:
This therapy(See stretching and strengthening exercises for Thoracic Outlet Syndrome) aims to reduce pressure on neurovascular structures through:
- Relaxation of the scalene muscles.
- Strengthening the muscles of the shoulders and shoulder girdle (trapezius, levator scapulae, SCM, pectorals, and suboccipital muscles).
- Postural exercises to correct poor posture.
Physical therapy is often combined with treatments such as hydrotherapy, massage, or pharmacological treatment (NSAIDs and muscle relaxants). Anesthetic blocks of the stellate ganglion or the scalene muscles have also been used.
Make an appointment with Dr. Jordi Jiménez. He will see you in the center of Palma and help you regain your quality of life.

![[VIDEO] Ultrasound-Guided Injection for Trigger Finger](https://drjordijimenez.com/imagen/100/100/Imagenes/infiltracion-ecoguidada-dedo-resorte-drjordijimenez.jpg)
![[VIDEO] Ultrasound-guided infiltration of the lumbar facets](https://drjordijimenez.com/imagen/100/100/imagenes-pagina/sindrome-facetario-lumbar-drjordijimenez (1).jpg)
![[VIDEO] Ultrasound-guided infiltration of the hip joint](https://drjordijimenez.com/imagen/100/100/Imagenes/valgo-dinamico-rodilla-drjordijimenez.jpg)