Calcific tendonitis of the rotator cuff
- 11/02/2019
What is calcific tendinitis or tendinosis of the shoulder?
Calcific tendinitis is a process in which intratendinous calcifications form. It is characterized by the deposition of calcium hydroxyapatite crystals within the tendon. It is a living, cell-mediated process that progresses over time and is self-limited. It can affect any tendon, with a preference for those without a synovial sheath: the FCU, finger extensors, or rotator cuff. Calcific tendinitis of the rotator cuff is a common condition in trauma clinics (10% of all consultations for shoulder pain). It is undoubtedly one of the most common causes of non-traumatic shoulder pain:
- The most affected tendon is the supraspinatus tendon, with a frequency ranging from 2.7% to 10%, depending on the series studied.
- It is a more common condition in women, especially those between the ages of 30 and 60.
- Bilateral involvement is present in 13–47% of cases.
- Diabetes mellitus is associated with up to 25%.
Why do calcifications form in the shoulder?
There are theories that attempt to answer why these calcifications form:
- Codman's degenerative theory: degenerative processes of tendon fibers would cause necrosis and dystrophic calcification.
- Uhthoff's calcific tendinitis theory: the calcification process would be cell-mediated, followed by a spontaneous phagocytic resorption process, unrelated to previous injuries, occurring at an early age and with spontaneous resolution.
In how many phases does a calcification form?
This accumulation of intratendinous calcium hydroxyapatite crystals occurs in three phases:
-Phase 1 or precalcification phase:
Often asymptomatic. Tendon degeneration and changes in the subacromiodeltoid bursa occur, predisposing to the second phase.

-Phase 2 or calcification:
Calcium pyrophosphate crystals accumulate, generating a significant inflammatory reaction, with inflammatory pain, generally unrelated to activity, more intense at night, and often interfering with the patient's rest.
-Phase 3 or post-calcification:
In which the calcium deposits may disappear through a resorption process.
What are the symptoms of calcific tendinitis of the shoulder?
The clinical presentation of calcific tendinitis varies widely. It may be an incidental finding in a patient seeking medical attention for another reason or be highly symptomatic with severe pain and significant functional limitations. Intrinsic factors that may influence the diagnosis include age and body mass index.
How is calcific tendinitis of the shoulder diagnosed?
The diagnosis is usually clinical: inflammatory pain unrelated to trauma or overexertion, present throughout the day but exacerbated at night. A plain X-ray confirms the diagnosis, and in our case, ultrasound is preferred to confirm the injury and determine the location (it avoids the radiation exposure caused by plain X-rays and CT scans).
How are calcifying tendinosis in the shoulder classified?
rom an ultrasound perspective, recent studies classify calcifications as granular (those with partially defined margins and irregular echogenicity), nodular (with a cystic appearance and sedimentary contents), and linear (thin and following the tendon course).
On the other hand, based on their density, they can be classified as:
- Type I or hard calcification: with a smooth, well-defined contour, a well-defined upper hyperechoic line, and a significant posterior acoustic shadow that obscures the cortical surface of the humerus. They are usually incidental findings without significant clinical manifestations, although they can, of course, be clinically significant.
- Type II or intermediate: with characteristics intermediate between types I and III, a less defined upper shadow and less acoustic shadow, so they subtly blur the humeral bone contour. They are usually more symptomatic than type I.
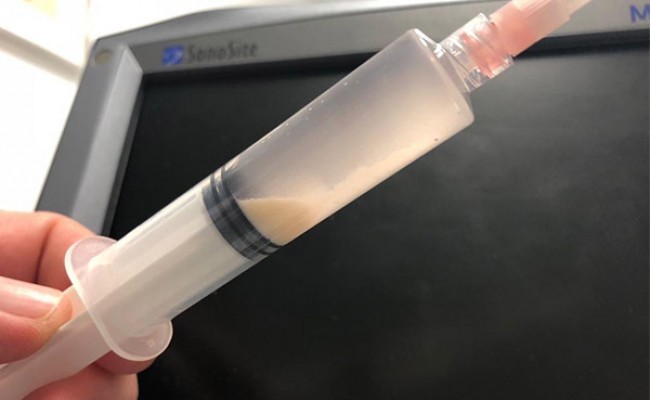
- Type III or soft: whose lumpy-pasty appearance gives them less hyperechogenicity and is less well-defined. They do not have acoustic shadowing. They are usually associated with the resorptive phase of calcification and are the most symptomatic.
What is the treatment for calcific tendinosis of the shoulder?
There are different treatments for calcific tendinosis of the shoulder:
- Initially, joint rest, analgesic-anti-inflammatory drugs, and exercises or rehabilitation regimens can improve the pain and prevent loss of mobility during the first few days.
- Shoulder therapeutic exercises: Once we've reduced the initial pain and maintained a mild level of pain, flexibility (stretching) and strengthening exercises maintain proper joint balance, preventing mobility reductions that can lead to adhesive capsulitis (frozen shoulder). See shoulder stretching and strengthening exercises.
- Cases resistant to these measures may be suitable for treatment with shock waves or ultrasound-guided therapies such as needle puncture lavage for thicker calcifications (type III) or barbotage in hard calcifications (type I).See article on barbotage:
- Surgical treatment will be reserved for cases in which all these measures fail to improve the clinical picture. We recommend arthroscopic debridement of the subacromial space and calcium deposits.See article on barbotage.
Make an appointment with Dr. Jordi Jiménez. He will see you in the center of Palma and help you regain your quality of life.

![[VIDEO] Ultrasound-Guided Injection for Trigger Finger](https://drjordijimenez.com/imagen/100/100/Imagenes/infiltracion-ecoguidada-dedo-resorte-drjordijimenez.jpg)
![[VIDEO] Ultrasound-guided infiltration of the lumbar facets](https://drjordijimenez.com/imagen/100/100/imagenes-pagina/sindrome-facetario-lumbar-drjordijimenez (1).jpg)
![[VIDEO] Ultrasound-guided infiltration of the hip joint](https://drjordijimenez.com/imagen/100/100/Imagenes/valgo-dinamico-rodilla-drjordijimenez.jpg)