Pectoralis minor syndrome
- 10/02/2023
What is pectoralis minor syndrome?
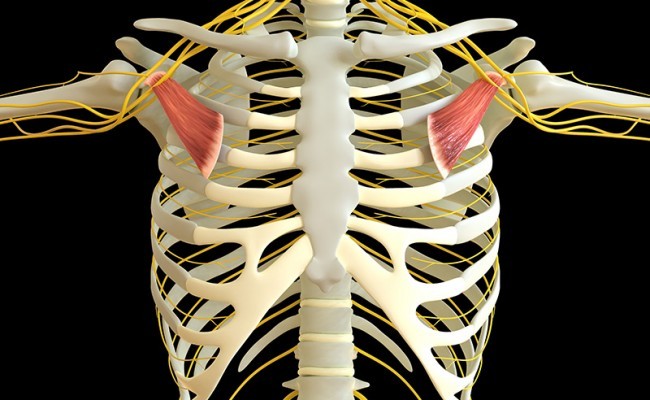
Pectoralis minor syndrome is a condition in which the pectoralis minor muscle, which is inserted between the scapula and the 3rd to 5th ribs, compresses nervous or vascular structures such as the brachial plexus, axillary artery, or axillary vein. Its stiffness, shortening, inflammation, or the presence of trigger points (contractures that occur within the muscle. See article on myofascial pain) can cause alterations in scapular mobility (scapular dyskinesis) and compression of these neurovascular structures.
Pectoralis minor syndrome is part of another syndrome, which we have already discussed (See article on thoracic outlet syndrome), in which compression of the brachial plexus occurs below the clavicle, specifically below the muscle's insertion on the coracoid process (scapula).
What are the causes of pectoralis minor syndrome?
The etiology of pectoralis minor syndrome is multifactorial and may include a combination of anatomical, postural, and overuse factors. Some of the factors that may contribute to its development include:
- Abnormal anatomy: Some people have anatomical variations in the muscle insertion that make them more prone to developing pectoralis minor syndrome.
- Improper posture: Maintaining an incorrect posture for a prolonged period of time or pre-established poor posture, with the shoulders excessively anterior, can increase tension in the pectoralis minor muscle and contribute to compression (See article on Janda's Upper Crossed Syndrome).
- Throwing sports that involve overhead arm activity, such as baseball, basketball, tennis, volleyball, handball, or swimming, can increase the risk of developing pectoralis minor syndrome.
- Strenuous physical activity: Weightlifting, swimming, and other strenuous sports can increase tension in the pectoralis minor muscle and contribute to its development.
- Repetitive trauma: These lead to the formation of tension and trigger points in the pectoralis minor muscle, which cause it to shorten and can increase the risk of developing pectoralis minor syndrome.
- Acute trauma: Neck hyperextension injuries, car accidents, and whiplash can cause pectoralis minor syndrome.
What are the symptoms of pectoralis minor syndrome?
The main diagnostic suspicion is neck and shoulder pain with paresthesia in one or both upper extremities, in which diagnostic tests do not clarify the pain radiating to the upper extremities (neck and shoulder MRI, electromyography do not clarify the pain pattern in the upper extremities). An important suspicious symptom is pain or tenderness upon palpation of the coracoid process (proximal insertion site of the pectoralis minor muscle).
Pain is usually the main symptom, located in the anterior shoulder, chest, neck, and arms, where numbness, numbness, and tingling may reach the 4th and 5th fingers. If there is compression of vascular structures, patients may complain of coldness in the affected arm or edema and swelling.
How is pectoralis minor syndrome diagnosed?
The diagnosis of pectoralis minor syndrome is made through a combination of clinical history, physical examination, and imaging tests. Diagnosis is often delayed and challenging for the specialist, given that the symptoms are common to other conditions such as nerve entrapment in the arm or neck problems. Some of the steps that can be taken to diagnose pectoralis minor syndrome include:
- Clinical history: The doctor will ask about the patient's symptoms, medical history, and lifestyle, including occupation, sports, and history of previous trauma. This is important if they participate in overhead sports (activity above the head) or work with repetitive elevation of the upper extremities.
- Physical examination: The doctor will perform a physical examination to assess strength, mobility, and sensation in the shoulder and arm. Diagnostic tests are available to reproduce the patient's painful symptoms. A positive Roos test is important (See article on thoracic outlet syndrome).
- Imaging tests: These are usually normal or do not explain the symptoms of pain radiating to the upper extremities. Imaging tests, such as X-rays, MRI, or CT, cannot confirm the diagnosis, but they can help rule out other causes of shoulder pain, neck pain, or pain radiating to the extremities.
- Electromyogram: Usually normal. Involvement of the medial cutaneous antebrachial nerve is highly suggestive of the diagnosis. It helps rule out other causes of pain radiating to the upper extremities that may coexist with pectoralis minor syndrome, such as peripheral neuropathies or cervical radiculopathies.
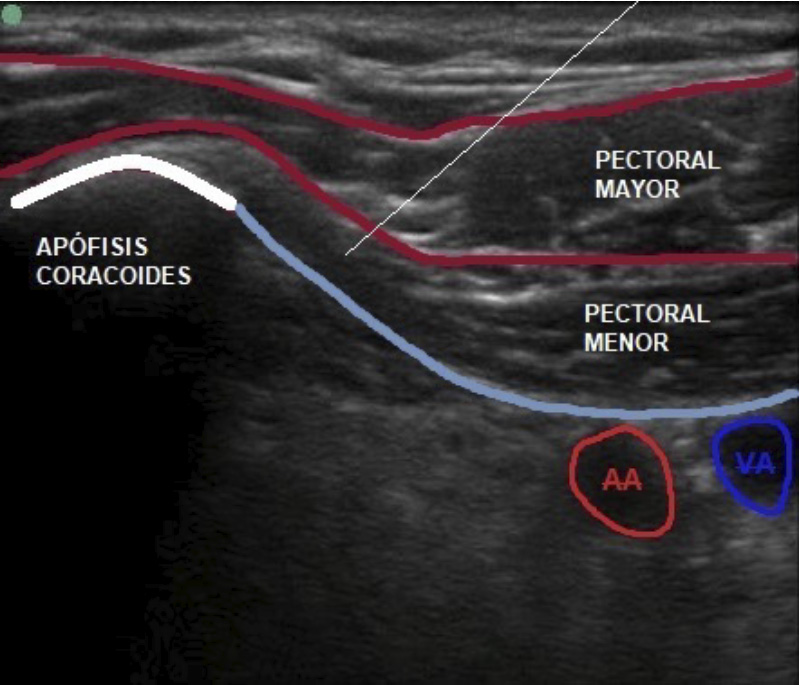
- Anesthetic blocks in the pectoralis minor muscle: Anesthetic blocks at the muscle level or blocks with botulinum toxin can confirm the diagnosis if there is clinical improvement with a re-evaluation of the Roos test after the block.
How is pectoralis minor syndrome treated?
Treatment for pectoralis minor syndrome depends on the severity of symptoms and the underlying cause. Some of the most common treatments include:
- Physical therapy: Physical therapy can help strengthen the shoulder muscles and correct posture. The therapist may also provide specific exercises to relieve tension in the pectoralis minor and improve mobility. Pectoralis minor stretches and postural correction are the cornerstone of rehabilitation treatment.(See stretching and strengthening exercises for Thoracic Outlet Syndrome)
- Manual therapy: Manual therapy, such as soft tissue manipulation, can help reduce inflammation and pain in the shoulder.
- Regulation and modification of activities of daily living: Modifying or avoiding certain activities that may be contributing to pectoralis minor syndrome can help relieve symptoms.
- Ultrasound-guided injections: Ultrasound-guided injections that combine anesthetics and corticosteroids can provide diagnostic guidance while simultaneously treating pectoralis minor pain.
In severe cases, a combination of treatments may be necessary to achieve significant improvement or, in more severe cases, surgery to treat symptoms.
Book an appointment with Dr. Jordi Jiménez. He will see you at the center of Palma de Mallorca and help you regain your quality of life.

![[VIDEO] Ultrasound-Guided Injection for Trigger Finger](https://drjordijimenez.com/imagen/100/100/Imagenes/infiltracion-ecoguidada-dedo-resorte-drjordijimenez.jpg)
![[VIDEO] Ultrasound-guided infiltration of the lumbar facets](https://drjordijimenez.com/imagen/100/100/imagenes-pagina/sindrome-facetario-lumbar-drjordijimenez (1).jpg)
![[VIDEO] Ultrasound-guided infiltration of the hip joint](https://drjordijimenez.com/imagen/100/100/Imagenes/valgo-dinamico-rodilla-drjordijimenez.jpg)