
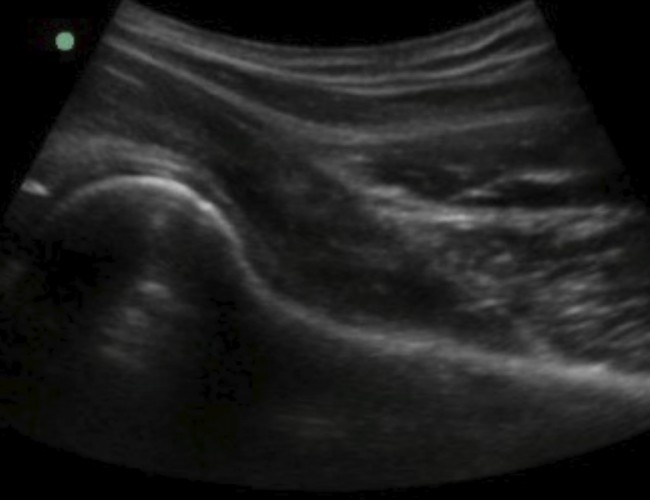
[VIDEO] Ultrasound-Guided Injection for Trigger Finger
- 18/11/2025
Trigger finger is a medical condition in which a finger gets stuck or locked in a bent position and then releases with a characteristic “click.” The condition can be painful and affect a person's ability to move the affected finger. It is more co...
.jpg)






















.jpg)






















































![[VIDEO] Ultrasound-Guided Injection for Trigger Finger](https://drjordijimenez.com/imagen/100/100/Imagenes/infiltracion-ecoguidada-dedo-resorte-drjordijimenez.jpg)
![[VIDEO] Ultrasound-guided infiltration of the lumbar facets](https://drjordijimenez.com/imagen/100/100/imagenes-pagina/sindrome-facetario-lumbar-drjordijimenez (1).jpg)
![[VIDEO] Ultrasound-guided infiltration of the hip joint](https://drjordijimenez.com/imagen/100/100/Imagenes/valgo-dinamico-rodilla-drjordijimenez.jpg)